Life is unpredictable, and medical emergencies can happen when least expected. In such moments, making critical healthcare decisions may not always be possible for an individual. This is where a medical power of attorney becomes essential, ensuring someone trusted can step in to make those decisions on their behalf.
A medical power of attorney is a legal document that grants a designated person the authority to make healthcare choices if the individual becomes incapacitated. This trusted representative, often called a healthcare proxy or agent, plays a crucial role in advocating for the person’s medical preferences.
Understanding how a medical power of attorney works and why it matters can empower individuals to take control of their future healthcare. It’s not just about planning for the unexpected—it’s about ensuring peace of mind for both the individual and their loved ones.
What Is Medical Power Of Attorney?
Medical power of attorney (MPOA) is a legal document that authorizes an individual, called the agent, to make medical decisions on behalf of another person, known as the principal. This authority becomes effective if the principal becomes unable to make healthcare decisions for themselves due to illness, incapacity, or unconsciousness.
The agent’s responsibilities can include consenting to or refusing medical treatments, selecting healthcare providers, and making decisions about living arrangements if they impact medical care. Agents must act in the principal’s best interests and, when possible, follow the instructions outlined in the MPOA or the principal’s advance directives.
State laws govern the creation and enforcement of MPOA documents, so requirements and terminology can vary. While some states refer to this role as a healthcare proxy or healthcare agent, the purpose remains consistent: to preserve the principal’s medical preferences during incapacitation.
Key Roles And Responsibilities
Agents under a medical power of attorney (MPOA) hold significant responsibilities to ensure the principal’s healthcare decisions align with their preferences when they’re unable to act for themselves. These roles require careful judgment and adherence to legal and ethical standards.
Decision-Making Authority
Agents possess the authority to make both routine and critical healthcare decisions on behalf of the principal. These decisions include consenting to medical treatments, declining procedures, or authorizing surgeries. This authority is activated only when the principal becomes incapacitated as confirmed by medical professionals. Agents are also tasked with coordinating with healthcare providers to execute these decisions.
Healthcare Preferences
Agents must follow the principal’s documented healthcare preferences as stated in the MPOA or advance directives. This includes decisions about pain management, recovery plans, and long-term care options, such as rehabilitation facilities or nursing homes. If preferences are not explicitly outlined, agents must act in the principal’s best interests using available information about their values.
End-Of-Life Decisions
In end-of-life scenarios, agents are responsible for making critical decisions about life-sustaining treatments, such as ventilators or feeding tubes. These choices must reflect the principal’s wishes, including preferences for hospice care or do-not-resuscitate (DNR) orders. Agents must ensure that the principal’s dignity and previously expressed intentions guide these decisions.
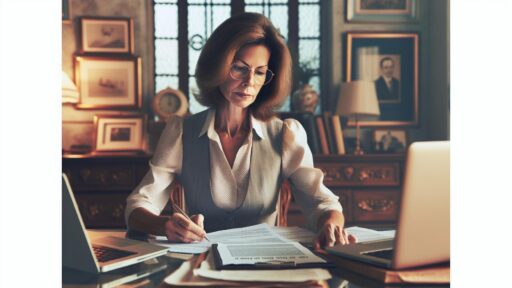
How To Choose The Right Agent
Selecting the right agent for a medical power of attorney ensures decisions align with the principal’s healthcare wishes. The agent plays a vital role in advocating for appropriate medical care during incapacitation.
Qualities To Look For
Look for individuals with reliability and the ability to make sound decisions under pressure. Agents should demonstrate good communication skills to interact with healthcare professionals effectively. Trustworthiness is essential to ensure the agent respects and follows the principal’s documented wishes. Emotional resilience matters since decisions may involve high-stress or end-of-life scenarios. Proximity can also be beneficial, as a local agent may respond faster during emergencies. Examples of ideal agents include close family members or long-term friends who understand the principal’s values.
Legal And Ethical Considerations
Agents must meet state-specific legal requirements, such as being of legal age, and avoid conflicts of interest. Some states prohibit appointing certain parties, like healthcare providers or employees of care facilities, as agents unless they are relatives. Ethically, they must prioritize the principal’s best interests and act within the scope defined by the MPOA. Instances of unethical behavior, like neglecting the principal’s directives, can lead to legal consequences or agent replacement. Confirming the agent’s willingness and ability to adhere to these responsibilities before appointment is essential.
Setting Up A Medical Power Of Attorney
Establishing a medical power of attorney ensures that healthcare decisions align with an individual’s preferences when they cannot make them independently. This involves understanding legal requirements and completing specific documents and processes.
Legal Requirements
Each state governs its own rules for medical power of attorney creation and execution. Generally, the principal must meet the legal age requirement, usually 18 or older, and possess the mental capacity to understand the document’s significance. The document must name a trusted agent and include specifics about their scope of authority. Depending on state laws, notarization or signatures from witnesses may be required to validate the MPOA. Some states restrict certain individuals, such as healthcare providers directly involved in the patient’s care, from serving as agents. Consulting an attorney familiar with local MPOA laws can help ensure compliance and accuracy.
Documents And Processes
Initiating the process requires obtaining an MPOA form, often provided by state agencies, legal services, or healthcare organizations. The form must clearly state the principal’s healthcare preferences and the agent’s authority. Drafting the document in alignment with any existing advance directives or living wills eliminates inconsistent instructions. After completing the form, the principal signs the document in the presence of an online notary or witnesses, as mandated by state laws. Once validated, copies of the MPOA should be distributed to the agent, healthcare providers, and trusted family members for accessibility during emergencies. Reassessing the document periodically allows for necessary updates in response to changes in the principal’s preferences or agent availability.
Benefits Of Having A Medical Power Of Attorney
Having a medical power of attorney (MPOA) provides critical advantages in situations where an individual cannot make healthcare decisions independently.
- Ensures Healthcare Preferences Are Respected
An MPOA guarantees that medical decisions align with the principal’s specified preferences. When outlined in advance directives or the MPOA, instructions regarding treatments, life-sustaining measures, or pain management can be upheld. - Provides Peace of Mind
Knowing that a trusted individual will advocate for their care relieves the principal and loved ones from uncertainty. It removes guesswork during emergencies, fostering confidence in decision-making. - Facilitates Timely Medical Decisions
An agent under an MPOA can make prompt decisions without needing court appointments or legal interventions. This is critical during emergencies when delays could risk the principal’s health or safety. - Protects Against Conflicts Among Family Members
By designating a single agent, an MPOA reduces the likelihood of disagreements among family members regarding medical care. Clear authority prevents confusion and ensures decisions align with the principal’s wishes. - Adapts To Unforeseen Circumstances
An MPOA allows flexibility when unexpected medical conditions arise. The agent can interpret and act on the principal’s healthcare goals as closely as possible, even when situations weren’t specifically detailed. - Forms a Legally Binding Framework
An MPOA holds legal recognition, ensuring healthcare providers comply with decisions made by the agent. This legal safeguard reinforces the principal’s autonomy even when they cannot communicate.
Discover the Power of BlueNotary:
Integrate your Business, Title Company, or Law Firm to Satisfy your Customers and Decrease Turnaround
Get a document Notarized/Sign-up
Join the Free Notary Training Facebook Group
Conclusion
A medical power of attorney is a vital tool for ensuring healthcare decisions align with an individual’s values and preferences when they’re unable to advocate for themselves. By carefully selecting a trusted agent and adhering to legal requirements, individuals can secure peace of mind for themselves and their loved ones. Taking the time to establish an MPOA helps protect personal autonomy, fosters clear communication, and provides a reliable framework for navigating challenging medical situations with confidence.
Frequently Asked Questions
What is a Medical Power of Attorney (MPOA)?
A Medical Power of Attorney (MPOA) is a legal document that allows a trusted person (the agent) to make healthcare decisions on behalf of someone who is unable to do so due to incapacity or illness.
When does a Medical Power of Attorney become effective?
An MPOA becomes effective when the principal is deemed incapacitated by a medical professional and can no longer make their own healthcare decisions.
What responsibilities does the agent have under an MPOA?
The agent must make medical decisions in the principal’s best interest, including consenting to treatments, selecting healthcare providers, or deciding on life-sustaining measures based on the principal’s wishes.
How do state laws affect an MPOA?
State laws determine the requirements, enforcement, and specific terminology for creating an MPOA. Consulting an attorney ensures compliance with local regulations.
Who should I choose as my MPOA agent?
Choose someone you trust who understands your healthcare preferences, makes sound decisions under pressure, communicates well, and is emotionally reliable. Proximity to you can also be helpful during emergencies.
Do I need an attorney to set up an MPOA?
While not always required, consulting an attorney can ensure your MPOA complies with state-specific laws and covers all necessary legal and healthcare considerations.
What documents are needed to create an MPOA?
You need the state-specific MPOA form, a clear statement of your healthcare preferences, and may require notarization or witness signatures as per state laws.
Can the MPOA be updated or revoked?
Yes, you can update or revoke an MPOA at any time as long as you are mentally competent. Regularly reassess it to reflect changes in preferences or agent availability.
What are the benefits of having an MPOA?
An MPOA ensures your healthcare choices are respected, provides peace of mind, enables timely decisions in emergencies, and prevents conflicts among family members by designating a trusted agent.
Can family members challenge the agent’s decisions under an MPOA?
If the agent acts within the boundaries of the MPOA and in accordance with the principal’s documented wishes, their decisions are legally binding. Family members generally cannot override them.